Table of Contents
Ayurveda treatment for Premature Ejaculation of Sperm

Premature Ejaculation of Sperm or early ejaculation, rapid ejaculation, rapid climax, premature climax, and (historically) ejaculatio praecox – refers to inability to last longer in sexual intercourse with your partner. Men’s typical ejaculatory latency is approximately 4–8 minutes. The opposite condition is delayed ejaculation. Men with premature ejaculation describe feeling that they have less control over ejaculating. This occurs when a man experiences orgasm and expels semen soon after sexual activity and with minimal penile stimulation.
Sex for humans is an expression of love, a sharing of intimacy, a form of communication, and often we feel it is an expression of our manhood or womanhood. However, it appears natural for a man to move toward vaginal intercourse, thrust upon penetration, and ejaculate quickly. The cause of PE could be temporary depression, stress, anxiety, a history of sexual repression, or a lack of emotional bonding between the partners. Physical disease can also be the reason, such as a swollen prostate gland (prostatitis), diabetes, sexually transmitted diseases, or cardiovascular disease.
- Biological and psychological factors can also play a role in causing premature ejaculation.
Psychological Factors
- Anxiety about intercourse,
- Being in a situation in which you hurry towards a climax,
- Cultural guilt related to sexual pleasure,
- Erectile dysfunction,
- Problems or lack of understanding between you and your partner,
Biological Factors
- Hormonal problems with the thyroid gland or abnormal levels of sexual hormones in the body,
- Problems with neurotransmitters in the brain, which therefore fail to carry right signals to the pleasure centers of the brain,
- Problems with the reflex mechanism of your ejaculatory system,
- Infection in the urethra or prostate,
- Heredity, and
- Damage to the nervous or sensory system due to either surgery or trauma.
- Some medications impair the reflex activity of your sexual organs. This means that while you are on these medications, you may have no control over your ejaculations.
- According to Ayurveda Premature ejaculation is caused by aggravation of Vata and Pitta Dosha.
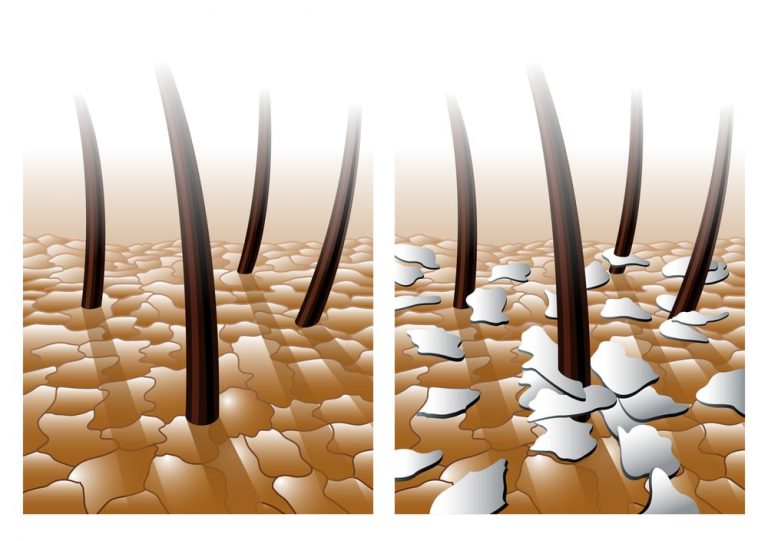
- These aggravated doshas cause hyperactivity of muscles in the male organ, thus increasing sensitivity to vibration
- Vata is characterized by its qualities of quickness and heightened sensitivity to the sense of touch. This gives a predisposition towards quicker ejaculation.
- According to Ayurveda Shukra dhatu (semen) is similar to purified butter. when there is Pitta (fire) aggravation in the body.
- Aggravated Pitta travels into the channels carrying semen, causing semen to decrease in consistency(thinning), and thus it gets ejaculated before sufficient erection. Just as purified butter melts in the presence of heat. Thus semen loses its consistency
Ayurvedic Treatment for Premature Ejaculation of Sperm
Ayurvedic treatment of premature ejaculation is mainly aimed at 3 thrings:-
- Pacifying the Vitiated Apana Vata
- Treating the Vitiated Pitta
- Providing medicines which can alter the sperm quality and and act as an aphrodisiac.
- Providing Medicines with Sthambana action
- Biological and psychological factors can also play a role in causing premature ejaculation.
Psychological Factors
- Anxiety about intercourse,
- Being in a situation in which you hurry towards a climax,
- Cultural guilt related to sexual pleasure,
- Erectile dysfunction,
- Problems or lack of understanding between you and your partner,
Biological Factors
- Hormonal problems with the thyroid gland or abnormal levels of sexual hormones in the body,
- Problems with neurotransmitters in the brain, which therefore fail to carry right signals to the pleasure centers of the brain,
- Problems with the reflex mechanism of your ejaculatory system,
- Infection in the urethra or prostate,
- Heredity, and
- Damage to the nervous or sensory system due to either surgery or trauma.
- Some medications impair the reflex activity of your sexual organs. This means that while you are on these medications, you may have no control over your ejaculations.
- According to Ayurveda Premature ejaculation is caused by aggravation of Vata and Pitta Dosha.
- These aggravated doshas cause hyperactivity of muscles in the male organ, thus increasing sensitivity to vibration
- Vata is characterized by its qualities of quickness and heightened sensitivity to the sense of touch. This gives a predisposition towards quicker ejaculation.
- According to Ayurveda Shukra dhatu (semen) is similar to purified butter. when there is Pitta (fire) aggravation in the body.
- Aggravated Pitta travels into the channels carrying semen, causing semen to decrease in consistency(thinning), and thus it gets ejaculated before sufficient erection. Just as purified butter melts in the presence of heat. Thus semen loses its consistency
Ayurvedic Treatment for Premature Ejaculation of Sperm:-
Ayurvedic treatment of premature ejaculation is mainly aimed at 3 thrings:-
- Pacifying the Vitiated Apana Vata
- Treating the Vitiated Pitta
- Providing medicines which can alter the sperm quality and and act as an aphrodisiac.
- Providing Medicines with Sthambana action
Internally
Arishta prepared with drugs like :- Chitraka, Pushkaramoola, Lodhra, Guduchi, Dhatri, Duralabha, Khadira, Asana, Pathya, Kushta, Manjishta, Dashamoola, Devadaru, Vidanga, Madhuka, Bharangi, Kapitha, Vibheethaka, Punarnnava, Chavya, Mamsi, Priyangu, Sariba, Krishna Jeeraka, Trivrt, Rasna, Pippali, Sati, Haridra, Shatapushpa, Shatahwa, Pathmaka, Nagakesara, Mustha, Yava, Srngi, Chandana, Jatiphala. Can alter the Sperm quality and consitency
Kashaya prepared with drugs like:- Rasna, Eranda, Vacha, Guduchi, Sahachara, Chavya, Musta, Bharangi, Ajamoda, Duralabha, Yavana, Vidanga, Karkkkataka Srngi, Sunthi, Bala, Murva, Katurohini, Ativisha, Triphala, Pippali, Yava Kshara, Rakta Chandana, Aragwada, Katukaphala, Indrayava. Can alter the Sperm quality and consitency.
Asava Prepared with Drugs like- Usheera, Valaka, Musta, Gambhari, Padma, Priyangu, Padmaka, Lodhra, Manjishta, Pada, Tikta, Nyagrodha, Pippali, Parppata, Madhuka, Rasna, Patola, Kanchanara, Amra, Mocharasa, Dhataki, Draksha. Can act as Stambhana also Pacifies vitiated Pitta Dosha
Choorna Prepared with Drugs like:- Triphala, KanjanaKsheeri, Saptala, Neelini, Vacha, Trayanti, Hapusha, Tikta, Saindhava, Pippali. Can act as Stambhana also Pacifies vitiated Pitta Dosha
Choorna and Kashaya that can control Apana Vata Vitiation and other Aphrodisiac medicines should be in taken.
Proper Counselling etc to remove Psychological Problems
Choorna and Kashaya that can control Apana Vata Vitiation and other Aphrodisiac medicines should be in taken.
Proper Counselling etc to remove Psychological Problems
Avoid intake of pitta-aggravating foods like hot, penetrating, or excessively salty and spicy foods, as well as chilies, garlic, pickles, fermented and preserved foods.
Increase intake of foods that are sweet and have a cooling effect on the body, like milk, butter, purified butter, almonds, raisins, black gram, licorice and asparagus.